Dive Deep into Creativity: Your Ultimate Tumblr Experience Awaits
Pharmacology - Blog Posts
Pharmacology is going to kill me. I have an exam on Thursday that I know I'm not going to do the greatest on since I've just been very unmotivated the last 2 weeks. Now that I'm feeling good again I'm kicking myself for not trying harder 😭 how am I going to memorize all these drugs?!
I tried to make two oddly specific warning signs.

Revision of some notes on the grapefruit juice effect on drugs, because pulling up a wikipedia page in a room of doctors would be a mistake
Look at that nasty grapefruit too

It is my first time using hex graph paper in a good while so I’m making it a new “chemicals of interest” notebook.
I think it looks passable so far, though sometimes I include the hydrogens because it’s fun to draw on this.


Metabolites of Caffeine (at least to the best of my referencing ability)

Cytochrome P450 Inducers & Inhibitors
The main ones can be remembered using "CRAP GPs spend all day on SICKFACES.COM".
Cytochrome P450 Inducers
These induce CYP450 activity, and thus reduce the concentration of drugs which are metabolised by this system.
Carbemazepine Rifampicin Alcohol (chronic use) Phenytoin Griseofulvin Phenobarbitone Sulphonylureas, St John's Wort, Smoking
Also topiramate.
Cytochrome P450 Inhibitors
These inhibit CYP450 enzyme activity and thus increase the concentration of drugs which are metabolised by this system.
Sodium valproate Isoniazid Cimetidine Ketoconazole Fluconazole Alcohol (acute use), Amiodarone, Allopurinol Chloramphenicol Erythromycin Sulfonamides, SSRIs Ciprofloxacin Omeprazole Metronidazole
Also grapefruit, cranberry juice, diltiazem, verapamil, clarithromycin.
Common Interactions
Medications which commonly interact with CYP450 inhibitors and inducers are:
Warfarin
Phenytoin
Combined Oral Contraceptive Pill (COCP)
Theophylline
Corticosteroids
Tricyclic antidepressants
Statins
Lamotrigine
Midazolam
Causes of drug-induced lupus
SHIP
Sulfasalazine & Sulfonamide Hydralazine Isoniazid Procainamide & Phenytoin
This is by no means a definitive list (they are many!) but these are some of the most common causes.
Common ototoxic medications
"FAV Q&A"
Furosemide (and other loop diuretics) Aminoglycosides Vancomycin Quinine Aspirin
Basic pharmacology of neuromuscular junction
ACh acts on N2 receptors (ligand-gated Na+/K+ receptors)
Block Na+ channels that propagate nerve impulse - local anaesthetics (lidocaine), tetrodotoxin
Inhibit ACh release - tetanus toxin, botulinum toxin
Competitive antagonists - vecuronium
N2 agonists - suxamethonium
Flaccid paralysis
Only cleared by plasma cholinesterase
Reversible anticholinesterases - edrophonium, neostigmine, physostigmine
Block activity of AChE
Diagnose and treat myasthenia gravis and treat glaucoma respectively
Irreversible anticholinesterases - organophosphates (pesticides, nerve gases)
Long-lived flaccid paralysis
Treat with pralidoxime within 10 minutes - cleaves OP-AChE complex
Management of acute MI
Reduce anginal pain
Morphine (+ anti-emetic)
Oxygen
Nitrate
Initiate reperfusion
Anti-platelet (aspirin, clopidogrel)
Thrombolytic (rtPA)
Primary angioplasty (PTCA)
Anticoagulant (heparin)
Protect myocardium
Beta-blocker
ACE inhibitor
Secondary prevention
Aspirin
Lipid-lowering (statin)
Lifestyle

Helpful mnemonic foe MI treatment.
What is Anemia of Chronic Disease?

Anemia of Chronic Disease (ACD), also known as anemia of inflammation or anemia of inflammation and chronic disease, is a prevalent condition often associated with chronic illnesses that last longer than three months and cause sustained inflammation. This form of anemia is particularly challenging because it not only stems from the chronic disease itself but also exacerbates the overall health burden on affected individuals.
Pathophysiology
The pathophysiology of ACD is closely linked to the body’s inflammatory response. Chronic inflammation, which is a hallmark of many autoimmune diseases and long-term illnesses, significantly alters iron metabolism. Normally, iron is recycled from old red blood cells and used in the production of new ones. However, in ACD, inflammatory cytokines, particularly interleukin-6 (IL-6), stimulate the production of hepcidin, a hormone that regulates iron homeostasis. Hepcidin inhibits iron absorption in the gut and traps iron in macrophages, making it unavailable for red blood cell production, leading to a functional iron deficiency. Additionally, chronic inflammation can suppress erythropoiesis (the production of red blood cells) and reduce the lifespan of existing red blood cells, compounding the severity of anemia.
Epidemiology and Affected Populations
ACD is the second most common type of anemia after iron-deficiency anemia, particularly in populations over the age of 65. It is often seen in individuals with chronic conditions such as cancer, chronic kidney disease (CKD), heart failure, and a range of autoimmune diseases including rheumatoid arthritis, systemic lupus erythematosus (SLE), and inflammatory bowel diseases like Crohn’s disease and ulcerative colitis. The prevalence of ACD in these populations highlights the importance of understanding and managing this condition effectively to improve overall patient outcomes.
Clinical Presentation
The clinical symptoms of ACD are often subtle and can overlap with those of the underlying chronic disease. Common symptoms include fatigue, weakness, pallor, shortness of breath, and dizziness. These symptoms may be exacerbated during physical activity. However, the mild nature of ACD symptoms means that the condition is often underdiagnosed or attributed solely to the chronic disease without recognizing the contribution of anemia.
Diagnosis and Laboratory Findings
Diagnosing ACD involves a combination of clinical evaluation and laboratory testing. Blood tests are crucial for identifying the characteristic features of ACD, including low hemoglobin levels, normal or elevated serum ferritin (reflecting adequate iron stores), low serum iron, and low transferrin saturation. The reticulocyte count is typically low, indicating reduced erythropoiesis. In some cases, a bone marrow biopsy may be conducted to assess iron stores directly and rule out other causes of anemia.
Management and Treatment Strategies
The primary approach to managing ACD is to address the underlying chronic condition. Effective treatment of the chronic disease often leads to an improvement in anemia. However, in cases where the anemia is severe or the chronic disease is difficult to control, additional interventions may be necessary. These can include:
Erythropoiesis-Stimulating Agents (ESAs): Synthetic forms of erythropoietin (EPO) can be administered to stimulate red blood cell production. This is particularly useful in patients with chronic kidney disease or cancer, where endogenous EPO production is impaired.
2 .Iron Therapy: Although oral iron supplementation is typically less effective in ACD due to hepcidin-induced iron sequestration, intravenous iron therapy may be beneficial, particularly when combined with ESAs.
3 .Blood Transfusions: In cases of severe anemia, blood transfusions may be required to rapidly increase hemoglobin levels. However, this is generally considered a short-term solution due to the potential risks of iron overload and transfusion-related complications.
Prevention and Lifestyle Modifications
While ACD itself may not be preventable due to its association with chronic diseases, patients can take steps to support overall health and potentially mitigate the severity of anemia. A balanced diet rich in iron (from sources such as lean meats and dark leafy greens), folate, vitamin B12, and vitamin C can support healthy red blood cell production. Regular monitoring of iron levels and timely medical intervention are essential in managing ACD effectively.
In conclusion, Anemia of Chronic Disease is a complex condition that requires a broad approach to diagnosis and management. Understanding the interplay between chronic inflammation and iron metabolism is key to effectively treating this form of anemia. Through careful management of the underlying disease and appropriate use of adjunct therapies, healthcare providers can significantly improve patient outcomes and reduce the burden of this condition.
As academic students and researchers navigate the challenges of their assignments and research endeavors, Expert Academic Assignment Help stands ready to provide professional guidance and assistance. Whether you require support with assignment writing, research paper assistance, or essay help, our team of experts is dedicated to helping you achieve academic excellence. Reach out to us today at expertassignment46@gmail.com and let us support you on your academic journey. We wish you success and professional excellence.
How to Write a Case Study

The case study indulges into the ideal process of rehabilitating a semi-professional cyclist who underwent a traumatic transfemoral amputation due to a road traffic accident. This comprehensive analysis aims to shed light on the complexities of limb loss rehabilitation, emphasizing the importance of tailored interventions and evidence-based practice in optimizing outcomes for individuals facing similar challenges.
Client Characteristics

In this section, a detailed exploration of the patient’s background, lifestyle, and medical history provides crucial insights into his unique rehabilitation needs. Emphasis is placed on the impact of the accident on the patient’s physical and psychological well-being, as well as his aspirations for returning to an active lifestyle post-amputation.
The patient, a previously healthy 24-year-old male, was actively engaged in semi-professional cycling and held a physically demanding job at a bicycle shop. The road traffic accident resulted in a traumatic transfemoral amputation, significantly altering his physical capabilities and emotional state. His aspirations to return to his previous level of physical activity underscore the importance of addressing both the physical and psychological aspects of his rehabilitation journey.
Examination Findings
A thorough examination is conducted to assess the patient’s physical condition and identify areas of impairment resulting from the amputation. Objective measurements, including strength assessments and gait analysis, complement subjective reports of phantom limb pain and functional limitations, forming the basis for the subsequent formulation of a clinical hypothesis.
The examination reveals significant impairments in strength and mobility, as well as the presence of phantom limb pain, which negatively impacts the patient’s daily life and rehabilitation progress. These findings highlight the need for a comprehensive treatment approach that addresses both the physical and psychological aspects of the patient’s condition.
Clinical Hypothesis/Impression

Drawing on current research and clinical expertise, the clinical hypothesis focuses on addressing the patient’s complex pain experience and psychological distress following the amputation. The identification of neuropathic pain mechanisms and the potential efficacy of interventions such as mirror therapy and mental imagery inform the development of a tailored treatment plan aimed at promoting pain relief and enhancing functional recovery.
The clinical hypothesis highlights the importance of addressing the underlying causes of the patient’s pain and implementing evidence-based interventions to optimize his rehabilitation outcomes. By targeting both the physical and psychological aspects of his condition, the treatment plan aims to improve the patient’s overall quality of life and facilitate his successful return to daily activities.
Intervention
The intervention plan is majorly crafted to address the patient’s unique rehabilitation goals and challenges. A multi-disciplinary approach, incorporating pharmacological interventions, prosthetic care, and psychological support, is implemented to optimize outcomes and empower the patient in his journey towards recovery. Detailed descriptions of specific treatment modalities and their rationale are provided, highlighting the importance of individualized care and ongoing monitoring throughout the rehabilitation process.
The intervention plan includes a combination of pharmacological management, prosthetic fitting and training, and psychological support to address the patient’s physical and psychological needs. Each component of the plan is tailored to the patient’s specific goals and challenges, with regular monitoring and adjustments made to ensure optimal outcomes.
Outcome
Objective measures are used to track the patient’s progress and evaluate the effectiveness of the intervention plan. Significant improvements in pain management, functional mobility, and quality of life are observed over the course of treatment, with particular emphasis on the transformative impact of mirror therapy on the patient’s pain experience and overall well-being. The importance of ongoing follow-up and support is emphasized as integral to maintaining long-term gains and facilitating the patient’s successful reintegration into daily activities.
The patient demonstrates significant improvements in pain management, functional mobility, and overall quality of life following the implementation of the intervention plan. Objective measures, including pain intensity ratings and functional assessments, demonstrate tangible improvements in the patient’s physical and psychological well-being, highlighting the effectiveness of the multi-disciplinary approach employed in his rehabilitation.
Discussion
A comprehensive discussion examines the broader implications of the case study for physiotherapy practice, highlighting the importance of holistic rehabilitation approaches that address the complex interplay of physical, psychological, and social factors in individuals with limb loss. Key lessons learned from the case study, including the value of evidence-based practice and the need for ongoing collaboration between healthcare professionals, are discussed in relation to optimizing outcomes and promoting patient-centered care.
The discussion explores the broader implications of the case study for physiotherapy practice, emphasizing the importance of adopting a holistic approach to rehabilitation that addresses the complex needs of individuals with limb loss. By integrating evidence-based interventions and fostering interdisciplinary collaboration, healthcare professionals can enhance the effectiveness of rehabilitation interventions and improve outcomes for patients with limb loss.
Conclusion
In conclusion, the extended case study provides a detailed exploration of the rehabilitation journey of a semi-professional cyclist following a traumatic limb amputation. Through a comprehensive analysis of client characteristics, examination findings, intervention strategies, and outcomes, valuable insights are gained into the complexities of limb loss rehabilitation and the importance of personalized, evidence-based care in achieving optimal outcomes for individuals facing similar challenges.
The case study underscores the importance of adopting a holistic approach to rehabilitation that addresses the physical, psychological, and social aspects of limb loss by focusing on interventions to the unique needs of each patient and fostering interdisciplinary collaboration, healthcare professionals can optimize outcomes and improve the quality of life for individuals with limb loss.
As academic students and researchers navigate the challenges of their assignments and research endeavors, Expert Academic Assignment Help stands ready to provide professional guidance and assistance. Whether you require support with assignment writing, research paper assistance, or essay help, our team of experts is dedicated to helping you achieve academic excellence. Reach out to us today at expertassignment46@gmail.com and let us support you on your academic journey. We wish you success and professional excellence.
10 Simple Tips for Caring for Your Heart.

The heart, a tireless worker at the core of our well-being, demands our attention and care. As we navigate through Heart Health Month this February, let’s explore ten simple yet impactful tips to ensure our hearts thrive. These practices, ranging from physical activity to laughter and dental hygiene, collectively contribute to a holistic approach to cardiovascular wellness.
1.Cardiovascular Exercise: A Heart’s Best Friend
Engaging in regular cardiovascular or aerobic activities is fundamental for heart health. Following the American Heart Association’s recommendations of 75 minutes of vigorous exercise or 150 minutes of moderate-intensity exercise weekly can significantly boost cardiorespiratory fitness. Activities such as running, cycling, or brisk walking not only elevate heart rate but also enhance overall cardiovascular function. The rhythmic contraction and relaxation of muscles during exercise contribute to improved blood flow and reduced strain on the heart.
2.Embrace a Smoke-Free Lifestyle
Quitting smoking is a paramount step in safeguarding your heart. Smoking damages both the heart and blood vessels, escalating the risk of cardiovascular diseases. Additionally, avoiding second-hand smoke is crucial, as it has been linked to heart attacks and strokes. The harmful chemicals in tobacco smoke lead to the narrowing of blood vessels, increasing the workload on the heart and elevating the risk of high blood pressure.
3.Prioritize Quality Sleep
Adequate sleep, often underestimated, plays a pivotal role in heart health. With at least seven hours of nightly rest, blood pressure lowers, and the body undergoes essential repair processes. Research underscores the correlation between poor sleep and heightened risks of high blood pressure, subsequently increasing the likelihood of heart diseases. Establishing a consistent sleep routine and creating a conducive sleep environment are crucial steps in promoting optimal cardiovascular health.
4.Regular Checkups: A Heart-Healthy Habit
Consistent visits to the doctor for heart health checkups are essential. Assessing risk factors such as diet, blood pressure, cholesterol, and family history enables early detection and management of potential issues. A proactive approach to heart health empowers individuals to make informed lifestyle choices. Regular checkups also provide an opportunity for healthcare professionals to offer personalized guidance on maintaining heart health through tailored interventions.
5.Laughter: The Heart’s Natural Tonic
Laughing, whether through entertainment or social interactions, yields surprising benefits for the heart. The act of laughter reduces artery inflammation, lowers stress hormones, and increases levels of good cholesterol. Integrating humor into daily life becomes a delightful prescription for heart health. Laughter promotes the release of endorphins, the body’s natural feel-good chemicals, which contribute to overall well-being and stress reduction.
6.Dental Hygiene and Heart Connection
Surprising as it may seem, maintaining good dental hygiene contributes to heart health. Studies reveal a link between poor dental health and the presence of bacteria in the bloodstream, impacting heart valves. Simple practices such as regular brushing can significantly decrease the risk of cardiovascular disease. Furthermore, regular dental checkups not only preserve oral health but also serve as a preventive measure against potential cardiovascular complications.
7.Fuel Your Heart with a Healthy Diet
A heart-healthy diet rich in fruits, whole grains, vegetables, and legumes significantly improves blood pressure and cholesterol levels. Steering clear of salty foods and saturated fats is crucial, as they contribute to elevated blood pressure and increased bad cholesterol. Incorporating omega-3 fatty acids, found in fatty fish, flaxseeds, and walnuts, further supports heart health by reducing inflammation and promoting optimal functioning of blood vessels.
8.Maintaining a Healthy Weight: A Heart’s Delight
Striving for and maintaining a healthy weight is a powerful defense against heart disease and high blood pressure. A combination of a balanced diet, regular exercise, and mindful calorie intake promotes overall well-being and cardiovascular health. Excess weight puts additional strain on the heart, leading to conditions such as hypertension and diabetes. Adopting sustainable lifestyle changes, including portion control and regular physical activity, contributes to achieving and sustaining a healthy weight.
9.Hydration: The Heart’s Elixir
Staying adequately hydrated is a simple yet often overlooked aspect of heart care. Considering the heart’s continuous effort in pumping around 2,000 gallons of blood daily, increased water intake supports its optimal functioning. Dehydration can lead to thicker blood, making the heart work harder to pump blood through the vessels. Maintaining proper hydration levels ensures the efficient transport of nutrients and oxygen to cells, promoting overall cardiovascular health.
10.Stay Active, Break Inactivity
Combatting sedentary lifestyles is crucial in preserving heart health. Incorporating simple changes like taking the stairs, walking, playing with pets, or engaging in household chores helps keep the heart active, reducing the risk of cardiovascular diseases. Prolonged sitting has been associated with various health risks, including obesity and heart disease. Regular physical activity not only supports cardiovascular health but also contributes to weight management and overall well-being.
In conclusion, adopting these ten heart-healthy habits provides a comprehensive approach to cardiovascular wellness. Whether it’s the joyous act of laughter, the discipline of regular exercise, or the mindfulness of a balanced diet, each step contributes to the harmonious symphony of a healthy heart. As we celebrate Heart Health Month, let’s embrace these practices and gift our hearts the care they deserve. Through consistent efforts and lifestyle modifications, we can ensure that our hearts continue to beat with vitality and resilience.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact us at expertassignment46@gmail.com for professional assistance.
What Are The Stages of Fetal Growth During Pregnancy?

The development of a fetus during pregnancy is a complex and remarkable process, marked by significant changes and growth each month. This journey is typically divided into three stages known as trimesters, each lasting approximately three months. For Healthcare professionals we discuss fetal development in terms of weeks. Here’s a detailed overview of what entails during each month of pregnancy.
a) First Trimester

The first trimester of pregnancy encompasses weeks 1 through 12 and is characterized by the initial formation and rapid development of the embryo. This period is critical for establishing the foundation of the future baby’s organs and body systems. The first trimester is often associated with the onset of pregnancy symptoms, such as nausea, fatigue, and hormonal changes.
Month 1 (Weeks 1–4)
Weeks 1–2: The first two weeks of pregnancy are technically considered a preparatory period. During this time, the body releases hormones and prepares the uterus for a potential pregnancy. This period includes ovulation, where an egg is released from the ovary. If fertilization occurs, the zygote forms and marks the beginning of pregnancy.
Week 3: Fertilization occurs when a sperm cell meets the egg, creating a zygote. This single-celled entity undergoes rapid cell division as it travels down the fallopian tube towards the uterus.
Week 4: The zygote becomes a blastocyst, which is a cluster of cells that implants itself into the uterine lining. The amniotic sac and placenta begin to form, playing crucial roles in protecting and nourishing the developing embryo. By the end of this month, the blastocyst is about 2 millimeters long, roughly the size of a poppy seed.
Month 2 (Weeks 5–8)
The second month of pregnancy marks significant developmental milestones as the embryo transitions into more complex forms.
Week 5: The neural tube, which will become the brain and spinal cord, begins to form. The heart, initially a simple tube, starts to pulse, setting the stage for the development of the circulatory system.
Week 6: Limb buds appear, which will eventually become arms and legs. Structures for the ears, eyes, and mouth start to take shape. Blood cells begin to form, and circulation starts within the embryo.
Week 7: The process of ossification starts as bones begin replacing the soft cartilage, and the formation of the genitals commences. The embryo now resembles a tadpole due to its prominent tail.
Week 8: Major organs and body systems continue to develop. The hands and feet start to form web-like structures, and the umbilical cord, which provides nutrients and oxygen to the embryo, is fully developed. By the end of this month, the embryo, now referred to as a fetus, is about 0.5 to 1 inch long, similar to a black bean.
Month 3 (Weeks 9–12)
The third month of pregnancy is marked by significant growth and maturation of the embryo, transitioning into a more recognizable human form.
Week 9: Teeth and taste buds begin to form. The fetus starts developing muscles, and its body takes on a more human appearance, although the head remains disproportionately large.
Week 10: Limbs and digits are fully formed, and the external genitals start to develop, although they are not yet visible on an ultrasound. The placenta continues to grow, providing essential nutrients to the fetus.
Week 11: The fetus begins to move spontaneously, exploring its surroundings by opening and closing its fists and mouth. The bones harden, though the skin remains translucent. Facial features such as the nose and lips become more defined.
Week 12: All essential organs, limbs, bones, and muscles are present and will continue to mature and develop. The fetus is about 2.5 to 3 inches long, roughly the size of a plum. At this stage, the risk of miscarriage decreases significantly, and many women begin to feel relief from early pregnancy symptoms like morning sickness.
Second Trimester

The second trimester of pregnancy spans from weeks 13 to 26. This period is often considered the most comfortable phase of pregnancy as many early symptoms subside, and the risk of miscarriage decreases. The fetus undergoes significant growth and development, and the mother begins to feel fetal movements, known as quickening.
Month 4 (Weeks 13–16)
During the fourth month, the fetus continues to develop rapidly, and its features become more distinct.
Week 13: Vocal cords form, and the fetus’s head starts to grow proportionally to the rest of the body. The fetus begins to practice breathing movements by inhaling and exhaling amniotic fluid, which helps develop the lungs.
Week 14: The skin starts to thicken and fine hair, known as lanugo, begins to grow. The fetus can bring its fingers to its mouth and may start sucking its thumb. External genitals are fully formed, and fingerprints start to develop.
Week 15: The intestines and ears move to their final positions. The fetus practices more purposeful movements, such as thumb-sucking and smiling. The developing nervous system allows the fetus to respond to external stimuli, such as light and sound.
Week 16: The fetus can hear and respond to external sounds. Its eyes, although still closed, can perceive light. By the end of this month, the fetus is about 5 inches long and weighs around 4 ounces, comparable to an avocado.
Month 5 (Weeks 17–20)
The fifth month of pregnancy is marked by increased fetal activity and continued growth.
Week 17: Fat begins to accumulate under the skin, providing insulation and energy reserves. The fetus’s skin is covered with a protective coating called vernix, which prevents it from becoming chapped by the amniotic fluid.
Week 18: The fetus is covered in lanugo, which helps keep it warm and provides an additional layer of protection. The fetus starts to establish a sleep-wake cycle, and its movements become more noticeable to the mother.
Week 19: The fetus’s movements, including kicks and punches, become more frequent and noticeable. Unique fingerprints are fully formed, and the fetus may start to experience hiccups.
Week 20: Nails develop fully, and the sensory areas of the brain mature, allowing the fetus to respond more actively to its environment. By the end of this month, the fetus is about 9 to 10 inches long and weighs around 1 pound.
Month 6 (Weeks 21–24)
The sixth month of pregnancy is a period of significant development, particularly in the nervous and respiratory systems.
Week 21: Coordinated limb movements become more frequent, and the fetus’s bone marrow begins producing blood cells.
Week 22: The fetus’s grasping reflex strengthens, and it can touch its surroundings, including its own body and the umbilical cord. It can hear internal sounds, such as the mother’s heartbeat and external sounds, such as voices and music.
Week 23: The fetus’s viability outside the womb increases, though intensive medical care would be necessary if it were born prematurely. The fetus starts rapidly accumulating fat, which is essential for temperature regulation after birth.
Week 24: Lung development progresses, although the lungs are not yet mature enough for the fetus to breathe independently. The fetus is about 12 inches long and weighs around 2 pounds.
Third Trimester

The third trimester of pregnancy spans from weeks 27 to 40 and is characterized by rapid growth and final preparations for birth. During this period, the fetus gains weight quickly and undergoes the final stages of development necessary for survival outside the womb.
Month 7 (Weeks 25–28)
During the seventh month, the fetus continues to grow and develop reserves of body fat.
Week 25: Increased body fat makes the fetus’s skin less wrinkled and more plump. The nervous system matures rapidly, enhancing the fetus’s ability to respond to stimuli.
Week 26: Melanin production begins, contributing to the skin and eye color. The lungs start producing surfactant, a substance that helps the lungs function properly after birth.
Week 27: The fetus’s eyes open, and it develops eyelashes. The fetus begins to develop regular sleep and wake patterns, and its movements become more coordinated.
Week 28: The fetus may begin to position itself head-down in preparation for birth. By the end of this month, the fetus is about 14 to 15 inches long and weighs between 2 to 3 pounds.
Month 8 (Weeks 29–32)
The eighth month of pregnancy involves continued maturation and growth of the fetus, with a focus on brain development.
Week 29: The fetus’s movements become more distinct as space in the uterus becomes cramped. The brain develops rapidly, allowing the fetus to control its body temperature more effectively.
Week 30: The fetus’s brain continues to grow, and it can process information and respond to stimuli. The fetus begins to establish more distinct patterns of activity and rest.
Week 31: The fetus’s skin loses its translucency as fat accumulates beneath it. Most organs, except for the brain and lungs, are fully developed and ready for birth.
Week 32: The fetus is about 17 to 18 inches long and weighs up to 5 pounds. The brain continues to develop rapidly, and the fetus can hear and respond to a variety of sounds.
Month 9 (Weeks 33–36)
During the ninth month, the fetus continues to grow and mature, preparing for birth.
Week 33: The fetus’s bones harden, although the skull remains soft and flexible to facilitate passage through the birth canal.
Week 34: The protective vernix coating thickens, providing additional protection to the fetus’s skin.
Week 35: Brain growth continues, and the fetus’s brain is now capable of regulating essential body functions.
Week 36: The lanugo covering the fetus’s body begins to disappear, and hair growth occurs on the head. The fetus is about 17 to 19 inches long and weighs 6 to 7 pounds.
Month 10 (Weeks 37–40)
The final month of pregnancy is a period of final preparations for birth, with the fetus reaching full maturity.
Week 37: The fetus’s toenails reach the tips of its toes. It continues to gain weight rapidly, preparing for the energy demands of life outside the womb.
Week 38: The fetus’s weight gain continues, and it starts to shed the vernix coating. The fetus moves lower into the pelvis in preparation for birth.
Week 39: The fetus is considered full-term and continues to develop and gain weight. It measures about 18 to 20 inches long and weighs between 7 to 9 pounds.
Week 40: The fetus is ready for birth. Its organs are fully developed and capable of functioning independently. The fetus positions itself head-down in the pelvis, preparing for delivery.
Throughout pregnancy, the fetus undergoes substantial growth and development, preparing for the transition to life outside the womb. Regular monitoring and care by healthcare providers are crucial to ensure the health and well-being of both the mother and the fetus. This comprehensive journey from a single cell to a fully developed baby highlights the incredible complexity of human development.
Expert Academic Assignment Help specializes in supporting medical students to study fetal growth during pregnancy. Our assistance includes study materials, tutoring, assignment help, and exam preparation, ensuring students understand fetal development. We provide mentorship, empowering students to excel academically and become competent healthcare professionals. Email: expertassignment46@gmail.comac
How Does The Drug Got Excreted / Eliminated From The Body?

Drug excretion is an important process in pharmacology, encompassing the elimination of pharmaceutical substances from the body. While the ultimate elimination of all drugs is inevitable, the specific pathways involved can vary significantly. Some drugs undergo extensive metabolic transformations before being excreted, while others are expelled from the body in their original form.
The kidneys play a central role in excreting water-soluble substances, effectively filtering them from the bloodstream. Meanwhile, the biliary system handles drugs that remain unabsorbed from the gastrointestinal tract, providing an alternative route for elimination. Although excretion through auxiliary channels such as the intestines, saliva, sweat, breast milk, and lungs is typically minimal, certain volatile anesthetics and residual drug traces in breast milk can have notable impacts, particularly on vulnerable populations such as infants.
Renal excretion constitutes a significant portion of drug elimination, accounting for approximately 20% of the plasma that is filtered through the glomeruli. While most water and electrolytes are reabsorbed back into circulation, polar compounds like drug metabolites are excreted predominantly in urine. However, it’s important to note that renal excretion tends to decrease with age, necessitating careful dosage adjustments for elderly patients to mitigate potential adverse effects.
Numerous factors influence the process of renal excretion, including the extent of protein binding, the degree of drug ionization affecting reabsorption rates, fluctuations in urine pH that can alter excretion dynamics, and the impact of metabolic inhibitors on tubular secretion mechanisms.
Biliary elimination, on the other hand, occurs when drugs traverse the biliary epithelium via active transport mechanisms. However, this process is not without limitations, as transporter saturation can impose constraints on drug excretion rates. Typically, larger molecules containing polar and lipophilic groups are excreted through bile, while smaller molecules tend to favor renal elimination pathways.
In addition to renal and biliary routes, drugs may also be eliminated to varying extents through auxiliary pathways such as saliva, tears, feces, sweat, and exhalation. While the quantities eliminated through these routes are generally minimal, drug excretion in breast milk can pose significant concerns for lactating mothers, potentially exposing nursing infants to pharmacological agents.
Understanding the pharmacokinetic parameters governing drug excretion is paramount for optimizing therapeutic regimens and minimizing the risk of adverse effects. Key parameters include the rate of elimination, clearance, elimination rate constant, and biologic half-life for drugs undergoing first-order elimination kinetics.
In conclusion, drug excretion represents a broad process influenced by a myriad of factors, necessitating comprehensive consideration to ensure the safe and efficacious use of pharmacotherapy.
For medical students navigating the complexities of their studies, Expert Academic Assignment Help serves as a beacon of professionalism and expertise. With a steadfast dedication to excellence and competency, our team provides invaluable support and guidance tailored to your academic needs. Do not hesitate to reach out to us for assistance on your academic journey, email: expertassignment46@gmail.com
Your excellence our pride.
Gangrene

Introduction
Gangrene, a condition marked by tissue death due to insufficient blood flow or bacterial infection, poses significant risks to affected individuals. Understanding the complexities surrounding gangrene, including its symptoms, causes, diagnosis, treatment modalities, and preventive measures, is paramount for healthcare professionals and the general public alike. This comprehensive discussion aims into the aspects of gangrene, providing insights into its various dimensions and fostering awareness for timely intervention and improved patient outcomes.
Overview of Gangrene
Gangrene manifests when tissues are deprived of adequate blood supply, leading to necrosis or cell death. Whether triggered by compromised circulation or bacterial invasion, gangrene can affect diverse anatomical regions, from the extremities to internal organs. Diabetes, atherosclerosis, and other vascular disorders heighten susceptibility to gangrene, underscoring the importance of vascular health in mitigating its onset.
Symptoms of Gangrene

Recognizing the subtle yet ominous signs of gangrene is critical for timely intervention. Symptoms encompass a spectrum of manifestations, including changes in skin color, swelling, blister formation, intense pain followed by numbness, malodorous discharge, skin texture alterations, and coolness upon touch. Systemic indicators such as fever, tachycardia, and hypotension may herald severe infection or septic shock, necessitating urgent medical attention.
When to See a Doctor
Prompt medical evaluation is imperative upon the onset of persistent, unexplained pain coupled with skin discoloration, discharge, or trauma-related symptoms. Delayed intervention can exacerbate tissue damage and precipitate life-threatening complications, underscoring the urgency of seeking professional care without delay.
Causes of Gangrene

Gangrene can arise from a constellation of etiological factors, ranging from vascular insufficiency to microbial infiltration. Conditions like diabetes, atherosclerosis, traumatic injury, or surgical interventions predispose individuals to gangrene by compromising tissue perfusion or facilitating pathogen colonization. Various subtypes of gangrene, including dry, wet, gas, internal, Fournier’s, and Maloney's gangrene, exhibit distinct pathophysiological mechanisms and clinical presentations, necessitating tailored therapeutic approaches.
Diagnosis and Treatment

Accurate diagnosis of gangrene entails a special evaluation of clinical symptoms, medical history, and ancillary investigations such as imaging and laboratory tests. Treatment strategies aim to restore tissue perfusion, eradicate infection, and remove necrotic tissue. Antibiotics, hyperbaric oxygen therapy, and surgical interventions like debridement or amputation constitute cornerstone modalities, guided by the severity and anatomical extent of gangrene.
Doctors and Departments
A multidisciplinary approach involving primary care physicians, vascular surgeons, infectious disease specialists, and wound care experts is indispensable for comprehensive management of gangrene. Collaborative efforts encompass diagnostic precision, therapeutic synergy, and rehabilitative support, ensuring holistic care tailored to individual patient needs.
Prevention
Preventing gangrene necessitates proactive measures targeting predisposing factors and promoting vascular health. Effective strategies encompass glycemic control in diabetes, lifestyle modifications, smoking cessation vigorous wound care, and early recognition of ischemic or infectious triggers. Vigilant surveillance and timely intervention mitigate the risk of gangrene development, fostering tissue preservation and optimizing long-term outcomes.
Conclusion
Gangrene epitomizes a formidable clinical challenge leading to various approach consisting of prevention, early recognition, and prompt intervention. Heightened awareness of gangrene’s clinical spectrum, coupled with proactive measures targeting predisposing factors, is important for mitigating its morbidity and mortality. By fostering collaboration among healthcare providers and empowering individuals with knowledge and preventive strategies, we can confront the scourge of gangrene and safeguard tissue viability, thereby promoting optimal health and well-being for all.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact at expertassignment46@gmail.com for assistance.
The Endocrine System

Introduction
The endocrine system is a complex network containing a symphony of hormonal interactions crucial for maintaining physiological equilibrium. Comprising glands, organs, and tissues dispersed throughout the body, its influence allows various bodily functions, spanning from metabolism to reproduction and beyond. This topic endeavors to provide an in-depth exploration of the endocrine system, encompassing its anatomy, physiological functions, associated conditions, and strategies for proactive care. By indulging into this indispensable regulatory system, we aim to equip readers with a comprehensive understanding to prioritize their hormonal health effectively.
Anatomy of the Endocrine System
The anatomy of the endocrine system is contained by an array of specialized glands, organs, and tissues, each endowed with the capacity to synthesize and dispatch hormones into the bloodstream. Principal among these are:
Endocrine Glands: These specialized tissues, including the pituitary gland, thyroid gland, and adrenal glands, secrete hormones directly into circulation, exerting systemic effects.
Endocrine Organs: Organs such as the hypothalamus, pancreas, and reproductive glands contribute to hormonal regulation, interfacing closely with the nervous system to modulate physiological responses.
Endocrine-Related Tissues: Adjunct to traditional endocrine structures, adipose tissue, kidneys, and even the heart harbor the capability to produce hormones, further augmenting the system’s complexity and regulatory capacity.
Functions of the Endocrine System
The cardinal function of the endocrine system is hormone secretion, holding up varied network of intercellular communication. Hormones, acting as molecular messengers, traverse the bloodstream to target cells, eliciting diverse physiological responses.
Key functions include:
Metabolism Regulation: Hormonal content govern metabolic processes, dictating energy expenditure, glucose homeostasis, and lipid metabolism.
Homeostatic Control: Endocrine signaling regulates internal threshold, modulating blood pressure, fluid balance, and body temperature.
Development and Growth: Hormonal interplay underpins growth trajectories and developmental milestones, steering embryonic stages and pubertal maturation.
Sexual Function and Reproduction: Hormonal modulation governs reproductive physiology, controlling fertility, libido, and secondary sexual characteristics.
Neuroendocrine Integration: The endocrine system reveals intimately with the nervous system, harmonizing behavioral and physiological responses, including mood regulation and sleep-wake cycles.
Conditions and Disorders
A spectrum of endocrine-related ailments afflicts individuals, stemming from hormonal imbalances, glandular dysfunctions, or neoplastic proliferations. Noteworthy conditions encompass:
Diabetes and Metabolic Disorders: Spanning type 1 and type 2 diabetes, metabolic syndrome, and obesity, these conditions disrupt glucose homeostasis and metabolic equilibrium.
Endocrine Cancers and Tumors: Malignancies affecting endocrine tissues, including adrenal tumors, pituitary adenomas, and thyroid malignancies, necessitate specialized oncological management.
Thyroid Dysfunction: Hypo- and hyperthyroidism, thyroid nodules, and autoimmune thyroiditis typify prevalent thyroid disorders, precipitating diverse clinical manifestations.
Reproductive and Sexual Health Disorders: From polycystic ovary syndrome (PCOS) to erectile dysfunction, disruptions in reproductive hormone signaling manifest as infertility, menstrual irregularities, and sexual dysfunction.
Proactive Care and Health Maintenance
In fostering endocrine wellness, a holistic approach integrating lifestyle modifications and environmental awareness is imperative. Strategies for promoting endocrine health encompass:
Lifestyle Optimization: Embracing a balanced diet, regular exercise regimen, and adequate sleep hygiene fosters metabolic resilience and hormonal equilibrium.
Environmental Vigilance: Mitigating exposure to endocrine-disrupting chemicals pervasive in everyday products, such as plastics, pesticides, and personal care items, reduces the risk of hormonal perturbations.
Health Surveillance: Individuals with familial predispositions to endocrine disorders benefit from proactive screening and vigilant symptom monitoring, facilitating early intervention and optimal disease management.
Conclusion
The endocrine entails physiological regulation, producing hormonal interactions essential for vitality and well-being. By looking at anatomy, physiological functions, associated conditions, and avenues for proactive care, this discourse endeavors to foster a comprehensive understanding of the endocrine system Empowered with knowledge, individuals can prioritize their hormonal health, embracing proactive measures to optimize their overall well-being and quality of life.
For medical students navigating the study of endocrinology and seeking guidance and academic support during their study period, Expert Academic Assignment Help offers invaluable assistance. With our expertise and resources, we provide tailored solutions to aid in comprehension, research, and academic success. Don’t hesitate to reach out to us for personalized assistance and elevate your understanding of this vital field. Your academic journey awaits, and we’re here to help you excel.
Contact us at expertassignment46@gmail.com for professional assistance,
Pulmonary Edema

Introduction
Pulmonary edema is a condition that results from the abnormal accumulation of fluid in the lungs, leading to impaired gas exchange and respiratory distress. This comprehensive discourse aims to provide an in-depth analysis of pulmonary edema, covering its pathophysiology, etiology, clinical manifestations, diagnostic modalities, treatment strategies, prevention strategies, and associated complications.
Pathophysiology of Pulmonary Edema

Pulmonary edema develops when there is an imbalance between the hydrostatic and oncotic pressures within the pulmonary vasculature. This imbalance leads to an increase in capillary permeability and the extravasation of fluid into the interstitial space and alveoli of the lungs. Several mechanisms contribute to this process, including increased capillary hydrostatic pressure due to heart failure, increased vascular permeability due to inflammation or injury, and decreased oncotic pressure due to hypoalbuminemia or capillary leak syndrome.
Etiology of Pulmonary Edema
The etiology of pulmonary edema can be categorized into cardiogenic and noncardiogenic causes. Cardiogenic pulmonary edema occurs secondary to heart failure or other cardiac conditions that result in elevated left atrial pressure and pulmonary venous congestion. Noncardiogenic pulmonary edema, on the other hand, is caused by factors unrelated to heart dysfunction, such as acute respiratory distress syndrome (ARDS), aspiration, sepsis, or neurogenic pulmonary edema.
Clinical Manifestations of Pulmonary Edema

The clinical presentation of pulmonary edema varies depending on the underlying cause and severity of the condition. Common symptoms include dyspnea, orthopnea, paroxysmal nocturnal dyspnea, cough, frothy sputum, cyanosis, and crackles on auscultation. Severe cases may progress to respiratory failure, hypoxemia, and hemodynamic instability.
Diagnostic Modalities for Pulmonary Edema

Diagnosing pulmonary edema requires a thorough clinical evaluation, including a detailed medical history, physical examination, and various diagnostic tests. Imaging studies such as chest X-ray, computed tomography (CT) scan, and lung ultrasound can provide valuable information about lung parenchymal changes and the presence of pulmonary congestion. Laboratory tests, including arterial blood gas analysis, brain natriuretic peptide levels, and electrolyte measurements, may also aid in the diagnosis and assessment of disease severity.
Treatment Strategies for Pulmonary Edema
The management of pulmonary edema involves addressing the underlying cause, relieving symptoms, and preventing complications. Initial treatment often includes supplemental oxygen therapy to improve oxygenation and reduce respiratory distress. Diuretics, such as furosemide or bumetanide, are commonly used to reduce fluid overload and alleviate pulmonary congestion. In cases of cardiogenic pulmonary edema, vasodilators, inotropes, or mechanical ventilation may be necessary to improve cardiac function and gas exchange.
Prevention Strategies for Pulmonary Edema
Preventing pulmonary edema requires a broad approach aimed at managing underlying risk factors and promoting healthy lifestyle habits. Patients with known cardiac conditions should adhere to prescribed medications, maintain a low-sodium diet, and monitor fluid intake to prevent fluid retention and exacerbation of heart failure. Individuals at risk of noncardiogenic pulmonary edema should avoid exposure to toxins, practice proper respiratory hygiene, and seek prompt medical attention for respiratory infections or injuries.
Complications of Pulmonary Edema

Untreated or inadequately managed pulmonary edema can lead to several complications, including acute respiratory distress syndrome (ARDS), cardiogenic shock, acute kidney injury, pulmonary hypertension, and death. Prompt recognition and intervention are essential to prevent progression to these life-threatening complications and improve patient outcomes.
Conclusion
Pulmonary edema is a complex and potentially life-threatening condition that requires prompt recognition, accurate diagnosis, and appropriate management. By understanding the underlying pathophysiology, etiology, clinical manifestations, diagnostic modalities, treatment strategies, prevention strategies, and associated complications of pulmonary edema, healthcare providers can optimize patient care and outcomes. Continued research efforts aimed at elucidating the mechanisms underlying pulmonary edema and identifying novel therapeutic targets are essential to further improve patient outcomes and reduce the global burden of this condition.
Embarking on your journey in the field of medicine is both exciting and challenging. As you navigate through your rigorous study period, it’s essential to seek guidance and assistance whenever needed to ensure your success.
At Expert Academic Assignment Help, we understand the demands of medical education and are here to support you every step of the way. Whether you require assistance with assignments, research papers, or exam preparation, our team of experts is dedicated to providing you with the help you need to excel in your studies.
Don’t hesitate to reach out to us for guidance, academic support, or any questions you may have. You can contact us via email at expertassignment46@gmail.com
What Is A Psychotic Disorders?

Introduction
Understanding psychotic disorders requires or encompassing various aspects such as types, symptoms, causes, diagnosis, treatment, prognosis, and preventive measures. Psychotic disorders constitute a diverse array of severe mental illnesses characterized by profound disturbances in cognition, emotion, communication, and behavior, significantly impairing individuals’ ability to function in daily life. Despite the gravity of these conditions, advancements in treatment modalities offer hope for recovery and effective management.
Types of Psychotic Disorders
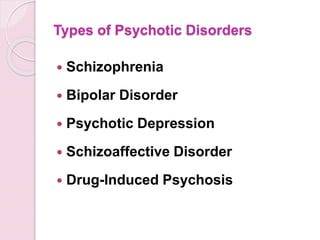
Schizophrenia
This debilitating disorder is characterized by profound alterations in behavior, delusions, and hallucinations persisting for at least six months. It exerts a profound impact on work, relationships, and overall functioning.
Schizoaffective Disorder
Combining features of schizophrenia with mood disorder symptoms like depression or bipolar disorder, schizoaffective disorder presents diagnostic and therapeutic challenges due to its complex symptomatology.
Schizophreniform Disorder
Resembling schizophrenia but with a shorter duration of symptoms (between one to six months), schizophreniform disorder provides insights into the acute phases of psychotic episodes.
Bipolar Psychotic Disorder
Individuals experience sudden, transient episodes of psychotic behavior, often precipitated by extreme stressors, with rapid recovery typically within a month.
Delusional Disorder
Centered around fixed false beliefs (delusions) concerning real-life situations, delusional disorder significantly influences perception and behavior, persisting for at least one month.
Shared Psychotic Disorder
Occurring when one individual’s delusion influences another within a close relationship, shared psychotic disorder elucidates the complexities of interpersonal dynamics in psychosis.
Substance-Induced Psychotic Disorder
Resulting from substance use or withdrawal, this condition underscores the intricate interplay between substance abuse and mental health.
Psychotic Disorder Due to Another Medical Condition
Hallucinations and delusions may arise secondary to underlying medical conditions affecting brain function, necessitating comprehensive evaluation and management.
Paraphrenia
Although not formally recognized in DSM-5, paraphrenia shares similarities with schizophrenia or delusional disorder and typically manifests in late adulthood, potentially associated with neurological factors.
Symptoms of Psychotic Disorders

Hallucinations
Involving perceptual experiences of stimuli that are not present in reality, hallucinations can manifest as auditory, visual, olfactory, gustatory, or tactile phenomena.
Delusions
These fixed, false beliefs persist despite evidence to the contrary, often revolving around themes of persecution, grandiosity, or paranoia.
Disorganized Thinking
Characterized by disjointed or incoherent thought processes, disorganized thinking manifests as impaired logical reasoning, tangential speech, or flight of ideas.
Bizarre Behavior
Individuals with psychotic disorders may exhibit unconventional or socially inappropriate behaviors, including agitation, catatonia, or unusual motor mannerisms.
Social Withdrawal
A hallmark feature of psychotic disorders is the withdrawal from social interactions and activities, often accompanied by a diminished interest in personal hygiene and self-care.
Mood Disturbances
Psychotic disorders may co-occur with mood symptoms such as depression or mania, further complicating the clinical presentation and treatment approach.
Causes of Psychotic Disorders

Genetic Predisposition
While genetic factors contribute to the risk of developing psychotic disorders, the inheritance pattern is complex, involving multiple genes and environmental interactions.
Environmental Factors
Stressful life events, trauma, childhood adversity, and substance abuse play significant roles in precipitating psychotic episodes and exacerbating symptoms.
Neurobiological Abnormalities
Dysregulation of neurotransmitters, particularly dopamine and glutamate, is implicated in the pathophysiology of psychotic disorders, affecting brain regions involved in cognition, perception, and emotion.
Diagnosis of Psychotic Disorders

A comprehensive diagnostic assessment involves obtaining a detailed medical and psychiatric history, conducting a thorough physical examination, performing laboratory tests to rule out medical conditions, and utilizing standardized psychiatric interviews and assessment tools.
Treatment of Psychotic Disorders

Medication
Antipsychotic medications are the cornerstone of pharmacological treatment, targeting symptoms such as delusions, hallucinations, and disorganized thinking. First-generation (typical) and second-generation (atypical) antipsychotics are prescribed based on efficacy and tolerability profiles, with newer agents offering improved side effect profiles and long-acting formulations enhancing treatment adherence.
Psychotherapy
Various forms of psychotherapy, including cognitive-behavioral therapy supportive therapy, and family therapy, complement pharmacotherapy by addressing psychosocial factors, enhancing coping skills, and improving functional outcomes.
Hospitalization
In severe cases or during acute psychotic episodes, hospitalization may be necessary to ensure safety, stabilize symptoms, and initiate intensive treatment interventions.
Prognosis and Recovery
The prognosis of psychotic disorders varies widely among individuals, influenced by factors such as early intervention, treatment adherence, social support, and the presence of comorbid conditions. While some individuals experience rapid symptom improvement and functional recovery, others may require long-term treatment and ongoing support to achieve stability and prevent relapse.
Prevention of Psychotic Disorders

Although prevention of psychotic disorders remains challenging, early intervention, identification of high-risk individuals, and mitigation of modifiable risk factors such as substance abuse and stress can reduce the incidence and severity of psychotic episodes. Public education, de stigmatization efforts, and access to mental health services promote awareness and facilitate timely intervention.
In conclusion, psychotic disorders represent complex and mental illnesses that profoundly impact individuals’ lives and necessitate comprehensive evaluation and treatment. By addressing the diverse array of symptoms, underlying neurobiological abnormalities, and psychosocial factors, clinicians can optimize treatment outcomes and support individuals in achieving improved quality of life and functioning. Through ongoing research, education, and advocacy, the understanding and management of psychotic disorders continue to evolve, offering hope for enhanced outcomes and reduced burden on affected individuals and society as a whole.
Students immersed in the fields of medical and psychology, seeking guidance from Expert Academic Assignment Help can be transformative. Whether it’s for assignments, studies, or navigating the challenges of medical School, expert assistance can provide clarity, direction, and invaluable insights. By reaching out to expertassignment46@gmail.com students can access personalized support, comprehensive resources, and expert advice to excel in their academic pursuits and lay a solid foundation for their future careers. Don’t hesitate to seek guidance — your academic success and professional growth are worth investing in.
Cirrhosis Of The Liver

Introduction
Cirrhosis stands as a challenge in the narrative of liver disease, marking the culmination of a complex interplay of factors that converge to undermine the organ’s structural integrity and functional capacity. This condition, characterized by the progressive accumulation of scar tissue within the liver parenchyma, holds a cascade of physiological network that reverberate throughout the body, manifesting in a spectrum of symptoms and complications. From its inner onset to its profound implications for morbidity and mortality, cirrhosis generate the intricate interplay between genetic predisposition, environmental influences, and individual behaviors.
In this comprehensive discussion, we embark on an exploration of the multifaceted dimensions of cirrhosis, traversing its etiological underpinnings, clinical manifestations, diagnostic modalities, therapeutic strategies, and avenues for prevention and self-care. By delving into the intricacies of cirrhosis, we endeavor to elucidate the imperative of early recognition, proactive intervention, and holistic management in ameliorating its adverse sequelae and fostering optimal outcomes for affected individuals
Pathophysiology of Cirrhosis

Central to the pathogenesis of cirrhosis lies a complex interplay of molecular and cellular events that precipitate the gradual transformation of healthy hepatic tissue into fibrotic scar tissue. At the heart of this process lies fibrogenesis, wherein a multitude of cellular players, including hepatic stellate cells, inflammatory mediators, and extracellular matrix proteins, triggers a profibrotic milieu in response to persistent liver injury and inflammation. The ensuing deposition of collagen-rich scar tissue disrupts the structure of the liver lobules, impeding normal hepatocellular function and vascular dynamics.
Symptoms and Clinical Manifestations

The clinical presentation of cirrhosis spans a broad spectrum, reflecting the diverse array of physiological derangements engendered by advanced liver disease. Early-stage cirrhosis may manifest subtly, with nonspecific symptoms such as fatigue, malaise, and vague abdominal discomfort, often eluding timely diagnosis. However, as the disease progresses, overt signs of hepatic decompensation emerge, including jaundice, ascites, hepatic encephalopathy, and gastrointestinal bleeding, heralding the onset of life-threatening complications. Moreover, cirrhosis exerts systemic effects beyond the confines of the liver, precipitating coagulopathy, renal dysfunction, and metabolic disturbances.
Etiology and Risk Factors
Cirrhosis arises from an influence of etiological insults, encompassing a diverse spectrum of predisposing factors that contribute to hepatocellular injury and fibrogenesis. Foremost among these is chronic alcohol abuse, which inflicts direct hepatotoxic effects and potentiates oxidative stress and inflammatory cascades within the liver microenvironment. Additionally, viral hepatitis infections, particularly hepatitis B and C, constitute major drivers of cirrhosis worldwide, underscoring the imperative of vaccination and antiviral therapy in disease prevention and management. Other contributing factors include nonalcoholic fatty liver disease, autoimmune disorders, hereditary hemochromatosis, and biliary tract diseases, each exerting a unique influence on cirrhosis pathogenesis.
Diagnostic Modalities

Accurate diagnosis forms the linchpin of effective cirrhosis management, necessitating a judicious amalgamation of clinical symptoms, laboratory investigations, imaging modalities, and histopathological evaluation. Liver function tests serve as indispensable tools for gauging the synthetic and metabolic capacity of the liver, while imaging studies such as ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) afford insights into hepatic morphology, vascular dynamics, and the presence of focal lesions. Despite their utility, these modalities may be supplemented by liver biopsy, which remains the gold standard for assessing the degree of fibrosis and guiding therapeutic decisions, albeit fraught with procedural risks and sampling variability.
Treatment Strategies

While cirrhosis represents a chronic and irreversible condition, therapeutic interventions are geared toward monitoring disease progression, alleviating symptoms, and forestalling the onset of complications. Pharmacological therapies, including hepatoprotective agents, antifibrotic agents, and symptom-based medications, aim to attenuate hepatic inflammation, inhibit fibrogenesis, and ameliorate symptom burden in cirrhotic patients. Furthermore, endoscopic interventions such as variceal band ligation and trans jugular intrahepatic portosystemic shunting play a major role in the management of portal hypertension and its sequelae, including variceal bleeding and refractory ascites. For select individuals with end-stage liver disease, liver transplantation offers a definitive therapeutic option, affording a second lease on life and circumventing the inexorable progression of cirrhosis-related complications.
Self-Care and Lifestyle

Empowering individuals with cirrhosis to adopt proactive self-care measures constitutes a cornerstone of comprehensive disease management, emphasizing the role of lifestyle modifications, dietary interventions, and preventive strategies in optimizing health outcomes. Lifestyle modifications, including abstinence from alcohol, adherence to a liver-friendly diet, regular exercise, and smoking cessation, are paramount in attenuating hepatic inflammation, promoting metabolic homeostasis, and mitigating cardiovascular risk factors in cirrhotic patients. Additionally, vaccination against hepatitis viruses, avoidance of hepatotoxic medications, and judicious monitoring of comorbid conditions serve as essential pillars of preventive care, safeguarding against disease exacerbations and fostering long-term wellness in individuals with cirrhosis.
Conclusion
Cirrhosis emerges as a complex and a dangerous disease, syndrome characterized by progressive hepatic fibrosis, compromised organ function, and a plethora of systemic manifestations. The etiological heterogeneity of cirrhosis underscores the need for a personalized and multidisciplinary approach to disease management, Focusing to the unique pathophysiological mechanisms and clinical manifestations inherent to each individual. Through timely diagnosis, targeted interventions, and collaborative care, healthcare providers can mitigate the burden of cirrhosis, optimize patient quality of life, and prolong survival in affected individuals. As we navigate complexities of cirrhosis, a concerted emphasis on preventive measures, patient education, and therapeutic innovations holds the key to unlocking a brighter prognosis for those afflicted by this formidable liver disease.
Medical students encounter significant academic challenges during their studies, balancing coursework, clinical rotations, research, and personal commitments. Expert Academic Assignment Help offers tailored assistance to meet their needs, providing study materials, tutoring, assignment help, and exam preparation. Beyond academics, it fosters a supportive environment for mentorship and guidance. In essence, Expert Academic Assignment Help is a valuable resource for medical students, empowering them to excel academically and develop into competent healthcare professionals. Contact at expertassignment46@gmail.com for assistance guidance.
How to Write a Case Study

Introduction
The case study indulges into the ideal process of rehabilitating a semi-professional cyclist who underwent a traumatic transfemoral amputation due to a road traffic accident. This comprehensive analysis aims to shed light on the complexities of limb loss rehabilitation, emphasizing the importance of tailored interventions and evidence-based practice in optimizing outcomes for individuals facing similar challenges.
Client Characteristics
In this section, a detailed exploration of the patient’s background, lifestyle, and medical history provides crucial insights into his unique rehabilitation needs. Emphasis is placed on the impact of the accident on the patient’s physical and psychological well-being, as well as his aspirations for returning to an active lifestyle post-amputation.
The patient, a previously healthy 24-year-old male, was actively engaged in semi-professional cycling and held a physically demanding job at a bicycle shop. The road traffic accident resulted in a traumatic transfemoral amputation, significantly altering his physical capabilities and emotional state. His aspirations to return to his previous level of physical activity underscore the importance of addressing both the physical and psychological aspects of his rehabilitation journey.
Examination Findings
A thorough examination is conducted to assess the patient’s physical condition and identify areas of impairment resulting from the amputation. Objective measurements, including strength assessments and gait analysis, complement subjective reports of phantom limb pain and functional limitations, forming the basis for the subsequent formulation of a clinical hypothesis.
The examination reveals significant impairments in strength and mobility, as well as the presence of phantom limb pain, which negatively impacts the patient’s daily life and rehabilitation progress. These findings highlight the need for a comprehensive treatment approach that addresses both the physical and psychological aspects of the patient’s condition.
Clinical Hypothesis/Impression
Drawing on current research and clinical expertise, the clinical hypothesis focuses on addressing the patient’s complex pain experience and psychological distress following the amputation. The identification of neuropathic pain mechanisms and the potential efficacy of interventions such as mirror therapy and mental imagery inform the development of a tailored treatment plan aimed at promoting pain relief and enhancing functional recovery.
The clinical hypothesis highlights the importance of addressing the underlying causes of the patient’s pain and implementing evidence-based interventions to optimize his rehabilitation outcomes. By targeting both the physical and psychological aspects of his condition, the treatment plan aims to improve the patient’s overall quality of life and facilitate his successful return to daily activities.
Intervention
The intervention plan is majorly crafted to address the patient’s unique rehabilitation goals and challenges. A multi-disciplinary approach, incorporating pharmacological interventions, prosthetic care, and psychological support, is implemented to optimize outcomes and empower the patient in his journey towards recovery. Detailed descriptions of specific treatment modalities and their rationale are provided, highlighting the importance of individualized care and ongoing monitoring throughout the rehabilitation process.
The intervention plan includes a combination of pharmacological management, prosthetic fitting and training, and psychological support to address the patient’s physical and psychological needs. Each component of the plan is tailored to the patient’s specific goals and challenges, with regular monitoring and adjustments made to ensure optimal outcomes.
Outcome
Objective measures are used to track the patient’s progress and evaluate the effectiveness of the intervention plan. Significant improvements in pain management, functional mobility, and quality of life are observed over the course of treatment, with particular emphasis on the transformative impact of mirror therapy on the patient’s pain experience and overall well-being. The importance of ongoing follow-up and support is emphasized as integral to maintaining long-term gains and facilitating the patient’s successful reintegration into daily activities.
The patient demonstrates significant improvements in pain management, functional mobility, and overall quality of life following the implementation of the intervention plan. Objective measures, including pain intensity ratings and functional assessments, demonstrate tangible improvements in the patient’s physical and psychological well-being, highlighting the effectiveness of the multi-disciplinary approach employed in his rehabilitation.
Discussion
A comprehensive discussion examines the broader implications of the case study for physiotherapy practice, highlighting the importance of holistic rehabilitation approaches that address the complex interplay of physical, psychological, and social factors in individuals with limb loss. Key lessons learned from the case study, including the value of evidence-based practice and the need for ongoing collaboration between healthcare professionals, are discussed in relation to optimizing outcomes and promoting patient-centered care.
The discussion explores the broader implications of the case study for physiotherapy practice, emphasizing the importance of adopting a holistic approach to rehabilitation that addresses the complex needs of individuals with limb loss. By integrating evidence-based interventions and fostering interdisciplinary collaboration, healthcare professionals can enhance the effectiveness of rehabilitation interventions and improve outcomes for patients with limb loss.
Conclusion
In conclusion, the extended case study provides a detailed exploration of the rehabilitation journey of a semi-professional cyclist following a traumatic limb amputation. Through a comprehensive analysis of client characteristics, examination findings, intervention strategies, and outcomes, valuable insights are gained into the complexities of limb loss rehabilitation and the importance of personalized, evidence-based care in achieving optimal outcomes for individuals facing similar challenges.
The case study underscores the importance of adopting a holistic approach to rehabilitation that addresses the physical, psychological, and social aspects of limb loss by focusing on interventions to the unique needs of each patient and fostering interdisciplinary collaboration, healthcare professionals can optimize outcomes and improve the quality of life for individuals with limb loss.
As academic students and researchers navigate the challenges of their assignments and research endeavors, Expert Academic Assignment Help stands ready to provide professional guidance and assistance. Whether you require support with assignment writing, research paper assistance, or essay help, our team of experts is dedicated to helping you achieve academic excellence. Reach out to us today at expertassignment46@gmail.com and let us support you on your academic journey. We wish you success and professional excellence.
H. pylori Infection

Introduction
Helicobacter pylori (H. pylori) infection is a significant global health concern, affecting a substantial portion of the world’s population. The discussion aims to provide an in-depth exploration of various aspects of H. pylori infection, including its prevalence, transmission, symptoms, diagnosis, treatment, complications, prevention strategies, and future research directions.
Prevalence and Transmission

H. pylori infection is widespread, with approximately two-thirds of the world’s population harboring the bacterium in their gastrointestinal tract. Various factors contribute to its prevalence, including socioeconomic status, living conditions, hygiene practices, and geographic location. The discussion indulges into the epidemiological trends of H. pylori infection across different populations and regions, highlighting disparities in prevalence rates and associated risk factors.
Transmission of H. pylori occurs primarily through interpersonal contact and ingestion of contaminated food or water. Saliva, fecal-oral transmission, and oral-oral transmission, including through kissing, are significant modes of spread. Poor sanitation and overcrowded living conditions facilitate the transmission of the bacterium, particularly in resource-limited settings. The discussion explores the mechanisms of H. pylori transmission and the implications for public health interventions aimed at reducing its spread.
Symptoms and Diagnosis

While many individuals with H. pylori infection remain asymptomatic, others experience a range of gastrointestinal symptoms, including stomach pain, bloating, nausea, and weight loss. The discussion elucidates the spectrum of clinical manifestations associated with H. pylori infection, emphasizing the importance of recognizing atypical presentations and considering differential diagnoses.
Diagnosing H. pylori infection presents several challenges due to the variability of symptoms and the limitations of available diagnostic tests. We critically evaluates the utility of different diagnostic modalities, including stool antigen tests, urea breath tests, and upper gastrointestinal endoscopy, in detecting H. pylori infection. It also examines the role of serological tests and molecular techniques in enhancing diagnostic accuracy and guiding clinical management decisions.
Treatment Options

The standard treatment regimens for H. pylori infection typically involve a combination of antibiotics and proton pump inhibitors (PPIs). However, rising rates of antibiotic resistance pose significant challenges to effective eradication therapy. It explores the mechanisms of antibiotic resistance in H. pylori and the implications for treatment outcomes.
Alternative treatment approaches, such as sequential therapy, concomitant therapy, and bismuth-based quadruple therapy, are also examined in the context of their efficacy and tolerability. Highlighting the importance of individualizing treatment regimens based on antibiotic susceptibility testing and patient-specific factors to optimize therapeutic outcomes.
Complications

Peptic ulcers are a common complication of H. pylori infection, resulting from the bacterium’s ability to disrupt the gastric mucosal barrier and induce inflammation. The discussion elucidates the pathophysiology of peptic ulcer formation and the factors contributing to ulcer recurrence and complications.
In addition to peptic ulcers, H. pylori infection is associated with an increased risk of more serious complications, such as gastric cancer and mucosa-associated lymphoid tissue (MALT) lymphoma. The discussion explores the molecular mechanisms underlying H. pylori-induced carcinogenesis and the strategies for early detection and management of gastric neoplasms.
Prevention

Preventive measures play a crucial role in reducing the burden of H. pylori infection and its associated complications. The discussion emphasizes the importance of promoting good hygiene practices, including handwashing and sanitation, to minimize the risk of transmission.
Furthermore, dietary factors may influence the risk of H. pylori infection and its clinical outcomes. The discussion evaluates the evidence regarding the impact of dietary habits, such as consumption of fruits, vegetables, and probiotics, on H. pylori colonization and disease progression. It also addresses the potential role of vaccination in preventing H. pylori infection and its complications, highlighting ongoing research efforts in vaccine development.
Research and Future Directions
Ongoing research efforts are focused on advancing our understanding of H. pylori pathogenesis, identifying novel therapeutic targets, and developing effective preventive strategies. The discussion highlights recent advancements in H. pylori research, including insights into bacterial virulence factors, host immune responses, and microbial interactions within the gastric microbiota.
Future directions in H. pylori research encompass a multidisciplinary approach, integrating molecular biology, epidemiology, immunology, and clinical medicine. The discussion outlines key areas for future investigation, such as the development of targeted antimicrobial agents, the role of host genetics in H. pylori susceptibility, and the impact of microbial dysbiosis on disease outcomes.
Conclusion
In conclusion, H. pylori infection remains a significant public health challenge, with implications for gastrointestinal health and disease worldwide. A comprehensive understanding of the epidemiology, pathogenesis, diagnosis, treatment, and prevention of H. pylori infection is essential for guiding clinical practice and informing public health policies. By addressing the complexities of H. pylori infection through interdisciplinary research and collaborative efforts, we can strive towards reducing its global burden and improving patient outcomes.
In managing H. pylori infection, compassion, empathy, and a holistic approach are crucial alongside clinical expertise. Striving for excellence in knowledge and practice enables us to advance gastroenterology and improve patient outcomes.
As we address H. pylori infection and its broader implications on gastrointestinal health, let’s remain dedicated to providing optimal patient care. By working collaboratively and embracing interdisciplinary approaches, we can positively impact lives and contribute to a healthier future.
Email expertassignment46@gmail.com to explore how we can assist you in achieving your academic and professional aspirations. Wishing you continued success in your medical journey.